Anatomy of Clinical Trial
Understanding how a vaccine goes from an idea to a product used to protect the public from infectious diseases
Each August we celebrate National Immunization Awareness Month. Throughout the month those of us in the medical and public health communities highlight the importance of vaccinations for all people of all ages.
Vaccines save lives.
In celebration of National Immunization Awareness Month — I am putting together a series of posts for the month of August focused on the history of vaccines, how the immune system works, the anatomy of a clinical trial (to test new vaccines), herd immunity, and three of my favorite vaccine-preventable disease.
The goal of this series (which will include new posts each Wednesday in August) is to educate you about the immune system & immunity, how vaccines are developed, and the diseases that vaccines prevent. And with the knowledge gained, I want to empower you to become fully vaccinated AND an advocate for vaccines in your community.
Here is part #3 in the series celebrating National Immunization Awareness Month — the ANATOMY OF A CLINICAL TRIAL
(Be sure to check out part #1 and part #2 in this series)
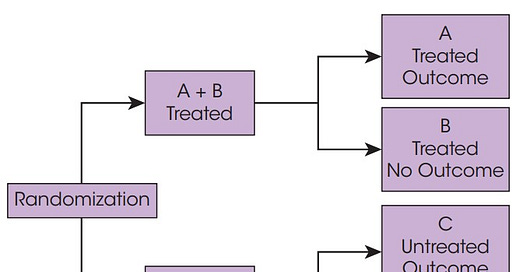
A clinical trial (aka a randomized clinical control trial) is a type of experimental epidemiological study in which the participants are placed (through a process called randomization, which will be discussed below) into an intervention/treatment group or a control/placebo group in order to evaluate the efficacy and safety of a new drug, medical device, or vaccine.
According to epidemiologist Dr. Leon Gordis (author of one of my favorite epidemiology textbooks) —
“The randomized trial is considered the ideal design for evaluating both the effectiveness and the side effects of new forms of intervention.”
At the beginning of a clinical trial, participants are randomized into either the intervention group, which receives the new drug, vaccine, or medical device. In the case of a vaccine clinical trial, individuals in the intervention group are given the new vaccine. Individuals not in the intervention group make up the control group. The control group receives either the standard of care — the best currently available intervention for the disease under study — or a placebo — a benign intervention designed to mimic the experimental intervention as closely as possible but does not contain the medication/vaccine. In the case of the COVID-19 vaccine trials, individuals in the control group received a shot of saline water. Therefore all of the study participants in the trial received two shots, either two doses of the vaccine or two shots of saline.
A process known as randomization is used to determine if a participant will be part of the intervention or placebo group. Randomization is a process by which participants have an equal probability or chance of being placed in the intervention or control group. Randomization can be done simply through a coin toss — everyone who flips a head is assigned to the intervention group; tales for the control group. Coins are not used for trials. We use random number generators or other online services that assign individuals to one group or the other. But the process of assigning individuals to either the treatment or control group is unbiased and usually blinded, meaning the participant (and often the team running the trial) does not know which group the participant has been assigned to.
The goal of randomization is to make sure the intervention and control groups are comparable. We want the groups to have a similar make-up in terms of factors that may impact the results of the trial, including gender, age, BMI, underlying health conditions, or previous illnesses.

In a clinical trial, participants are randomized to their group and then those participants are followed for a period of time to determine the outcome of the study, specifically, we measure each participant in both groups to determine if they become ill or develop antibodies (whatever the trial is studying).
In the case of the COVID-19 trials — individuals in both groups were followed to see if (1) they developed COVID-19 or not; (2) if they developed COVID-19, were they hospitalized or did they die; or (3) if they developed COVID-19 antibodies.
Researchers compare the number of outcomes that occurred in the control group to the number of outcomes that occurred in the treatment group. We measure the differences between the groups by calculating efficacy. Efficacy measures a reduction in risk in individuals who have received the vaccine as opposed to those who did not.

NOTE: despite the apparent similarity, the effectiveness of a vaccine refers to the ability of an intervention/vaccine to produce benefits (read: the vaccine works at preventing or mitigating disease) among those who were offered the vaccine in a real-world environment. Efficacy is what we measure in the trial. Effectiveness we measure in the real world among the general population.
In order for a new drug or vaccine to make it to the general public, it must undergo three clinical trial phases.

Throughout these phases, the safety and efficacy of the drug or vaccine are evaluated.
Individuals who believe that the COVID vaccines were developed too quickly often believe that too few individuals participated in the trial. For example, how can we be sure that the vaccine is safe and effective if the trial only included only 5,000 individuals? The reality is epidemiologists coordinating these trials are required to strike a very delicate balance… we need to include enough people to ensure that the results of the trial are generalizable/applicable to the general public. But we also do not want to subject more people than necessary to the risks associated with participating in a clinical trial (of an unapproved vaccine).
In order to strike this balance, we use statistical analyses to determine what sample size is necessary. The sample size is not determined willy-nilly. A lot of time is spent calculating the appropriate sample size for each phase of the trial.
An independent data-safety monitoring board (read: a group not involved in the administration or analysis of the trial results) monitors the health and safety of all of the participants in the trial. If members of the data-safety monitoring board believe that the health or safety of trial participants is jeopardized, they have the authority to stop the trial. The safety of individuals participating in the trial is of the utmost importance.
In the words of my previous boss at a pool where I worked as a lifeguard, we put —
“Safety first, first”
in a clinical trial.
We also use the best science and most sophisticated epidemiological and biostatistical techniques to ensure that we include enough people in a trial but do not over-enroll trials unnecessarily. There is nothing willy-nilly about a clinical trial. They are regulated and monitored closely to ensure the safety of participants and the development and correct dosing of drugs, vaccines, and medical equipment to improve the health of individuals throughout our communities.
Have more questions? Please ask me!
If you’d like to learn more, I recommend reading chapter 11 in the textbook I wrote Understanding Epidemiology. You can also learn more here.
And please remember, the clinical trial process described above has been used to approve vaccines for everything from polio to rotavirus, as well as chemotherapy treatments for cancer, artificial heart valves, and antibiotics used to cure people suffering from sepsis. Vaccines do not receive special treatment; they are held to the same high standards of review as all other medical interventions.