Given that we are living through THREE global health emergencies (COVID, polio, and monkeypox), new vaccines are being approved, new outbreaks are occurring, and the reality that being healthy is truly a radical selfless act of loving others (read: we need to redefine what it means to be healthy), “Three Things Thursday” highlights three things I am paying attention to as an epidemiologist each week. This week I’m focusing on three vaccines (it is National Immunization Awareness Month!!).
Hoping these posts help to educate and empower you to be healthy and create healthy communities.
Here we go… Three Things Thursday.
COVID Booster Shots
Everyone who is 5 years old or older is eligible for at least one booster shot of the COVID vaccine. And in light of the spread of various Omicron subvariants (BA.4, BA.5), a booster dose (or two depending on your age or health history) is needed. As I wrote yesterday, these new variants can sneak into our bodies and begin to replicate causing cell damage and cell death before the immune system can sound an alarm; the virus is evading key warning systems of our innate immune system. It is, therefore, absolutely necessary to be up to date on COVID vaccinations (and booster shots) so that your adaptive immune system has the memory and tools (COVID-specific antibodies) to fight a COVID infection once the virus is detected in your body.
Vaccinations are essential to prevent severe illness and death.
Many people have asked me if they should delay a booster shot now and wait for the new bivalent booster shots that are expected sometime this fall.
Should you wait? Absolutely, positively NO!
If you are eligible for a booster shot now, you should go get it NOW.
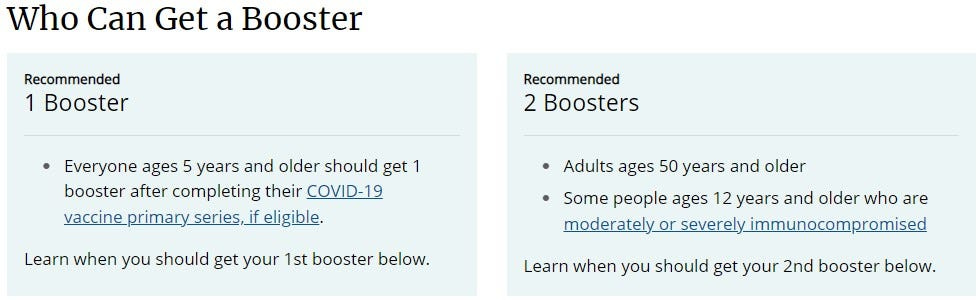
The boosters that are available now offer the best defense against COVID-19. And we are not expecting the new booster shots until October at the earliest. It could be December before they are widely available (assuming the clinical trial results show that the new boosters are more effective and as safe as the current booster doses).
Waiting for the new shots is a gamble. One NOT worth taking.
Additionally, it is worth noting that we cannot predict what the SARS-CoV-2 virus is going to do next. By the time the new booster shot (which will contain the mRNA from an Omicron subvariant), the virus may have mutated again and we may be facing a new variant altogether.
Getting boosted now is essential. Don’t wait. Don’t gamble. Don’t think it is unnecessary. Booster shots save lives.
Universal Influenza Vaccine Trial Begins
On Tuesday, the Journal of the American Medical Association (JAMA) reported that a Phase I clinical trial to investigate the safety and effectiveness of a “universal flu” vaccine candidate has begun. According to Dr. Anthony Fauci having influenza —
“vaccines that can provide long-lasting protection against a wide range of seasonal influenza viruses, as well as those with pandemic potential, would be invaluable public health tools.”
Prior to the start of the clinical trial, researchers studied the vaccine candidate in animals. They found that vaccinated mice and ferrets (which are commonly used as an animal model for human vaccine trials) survived lethal doses of six different strains of influenza. The Phase I trial was approved following the success of the animal trials.
A Phase I trial is the first of three phases in the clinical trial process and this phase aims to ensure that the vaccine is safe for humans. Additionally, during Phase I trials, researchers gather the first round of evidence regarding the efficacy of the vaccine. Phase I trials tend to be small, and the universal flu vaccine trial is no different. There are currently 100 healthy adults (18-55 years) participating in the trial. They will be followed for at least seven months.
Results of the trial should be available in early 2023…
Supply & demand for monkeypox vaccine
Monkeypox is a serious and fast-growing public health problem. Despite the fact that the majority of the spread is limited to specific social and occupational groups, we should expect (and already are seeing signs) that monkeypox is spreading throughout all of our communities.
Thankfully, monkeypox is a vaccine-preventable disease. And the vaccine can be given post-exposure (before symptoms develop).
HOWEVER, the supply of monkeypox vaccines (called Jynneos) is not keeping up with the demand. Approximately, 3.2 million Americans are at high risk of monkeypox and are being encouraged to get vaccinated now. However, there are only 1 million doses of Jynneos in the Strategic National Stockpile (SNS). And Bavarian Nordic, which manufactures Jynneos, isn’t expected to be able to meet the demand for the vaccine in the near future.
In response to the supply & demand problem, the US Government earlier this week approved a policy that would allow healthcare providers to reduce the dosage of the Jynneos vaccine — so that what was a single dose previously can now be split into five doses. Many people in the public health and medical communities are wondering if diluting the dosage will result in an effective vaccine.
It feels like a gamble, but more vaccine is needed.
There are also serious conversations occurring about using ACAM2000, the smallpox vaccine, in response to the monkeypox outbreak. There is some evidence that the smallpox vaccine will provide protection against monkeypox, and there are 100 million doses of ACAM2000 in the SNS.
Using the smallpox vaccine solves the supply problem,
BUT it opens up two new serious cans of worms —
First, will the smallpox vaccine provide enough protection to slow the spread of monkeypox and reduce the severity of the disease among individuals who are infected? In other words, will the benefits of the smallpox vaccine be worth the risks associated with the vaccine?
This leads us to the second can of worms… the smallpox vaccine contains a live, replication-competent vaccinia virus. Meaning it is a live virus vaccine, capable of causing vaccinia illness in individuals. NOTE: vaccinia is a milder pox virus. It is similar to smallpox, but not as lethal. Individuals vaccinated with the smallpox vaccine are required to cover and take care of the vaccination site for 2-6 weeks post-vaccination or else risk spreading the virus. Using the smallpox vaccine puts individuals with compromised immune systems at increased risk of developing a vaccinia infection.
There is no simple solution to the supply and demand problem associated with the monkeypox outbreak. And the costs and benefits of diluting vaccine doses or deciding to use the smallpox vaccine will be made in the coming months. NOTE - at this point in time I am not supportive of using the smallpox vaccine to curb the monkeypox outbreak. Other really smart people agree with me at this point in time. However, only time will tell if more vaccine is needed and if policymakers and the public alike can stomach a smallpox vaccination campaign.
Prevention of monkeypox is key.
And as our children, grandchildren, nieces, nephews, and family friends head back to school — it is essential that they are up to date on their vaccinations.